It becomes more common as we age, and is characterized by the sudden urgent need to urinate, even when the bladder isn’t full, resulting in patients rushing to the bathroom multiple times per day/night. This uncontrollable urge feeling is the telltale sign of OAB. Other symptoms may include urinary frequency (>8 trips to the bathroom), nocturia (multiple night-time bathroom visits), and urinary leaks otherwise known as urinary incontinence. 91% of patients are untreated and 68% of patients are undiagnosed, potentially believing a “weak bladder” is a normal part of aging– With NiNA*, it doesn’t have to be.1, 2, 3
Not to be confused with Stress Urinary Incontinence, which is caused by weak pelvic floor muscles (often a result of childbirth), OAB by contrast is a condition affecting the nerves that control the bladder. Some patients have both conditions. NiNA is intended for the treatment of OAB4.
People often spend more time confined to their homes, afraid to venture out for fear of embarrassing bladder accidents5. Functional impacts include missing work, sleep disturbance (from waking up repeatedly to go to the bathroom), urinary tract infections (UTIs), and falls & fractures that result from patients running to the bathroom. Incontinence is one of the leading causes of admission to assisted living facilities6,7. One study puts the total economic impact of OAB at $82B, including 75% in direct spend8,9.
NiNA has the opportunity to vastly improve quality of life for these patients– many of whom are silently suffering with diapers and pads.
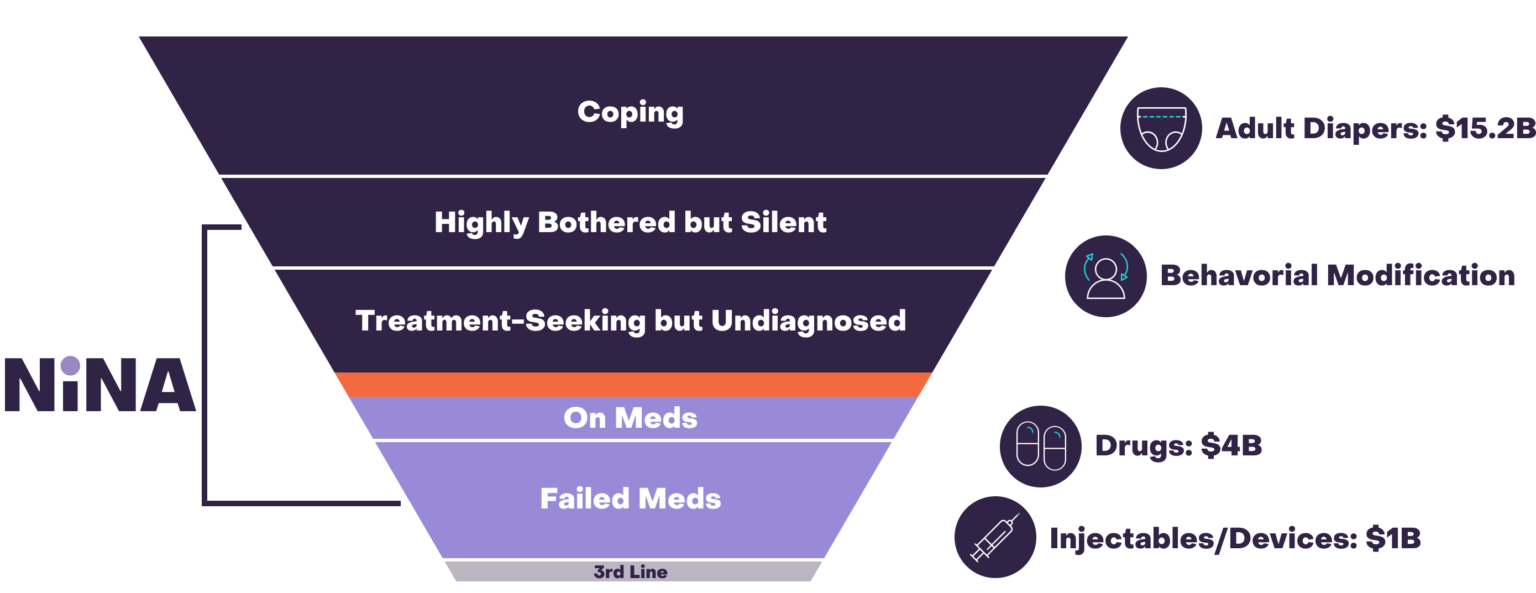
Adult diapers and incontinence pads are commonly used but don’t address the cause of OAB, and can sometimes result in painful recurrent urinary tract infections. Medications are linked to a host of side-effects including dry-mouth, dizziness, fatigue, hypertension, and constipation. Approximately 80% of patients discontinue medications after 6 months, mainly due to side-effects10. Lastly, third-line therapies like PTNS, SNS, and botulinum toxin, while proven, are invasive, require clinic visits, have numerous significant side effects, and are expensive. NiNA is being designed to work as an alternative to medications early in patients’ journey, potentially with better efficacy than medications.
Enormous opportunity for a product without the risk of surgery or side effects of drugs to disrupt and expand the market.
1Stewart, W. F., et al. (2003). Prevalence and burden of overactive bladder in the United States. World Journal of Urology, 20(6), 327–336.
2Benner, J. S., et al. & OAB Medication Use Study Steering Committee (2009). Bother related to bladder control and health care seeking behavior in adults in the United States. The Journal of Urology, 181(6), 2591–2598.4
3Duralde, E. R., et al. (2016). Bridging the gap: determinants of undiagnosed or untreated urinary incontinence in women. American journal of obstetrics and gynecology, 214(2), 266.e1–266.e9.
4Altman, D., et al. (2006). Risk of urinary incontinence after childbirth: a 10-year prospective cohort study. Obstetrics and gynecology, 108(4), 873–878.
5Hawkins, K., et al. (2011). The prevalence of urinary incontinence and its burden on the quality of life among older adults with medicare supplement insurance. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation, 20(5), 723–732.
6Gaugler, J. E., et al. (2007). Predicting nursing home admission in the U.S: a meta-analysis. BMC geriatrics, 7, 13.
7Morrison, A., & Levy, R. (2006). Fraction of nursing home admissions attributable to urinary incontinence. Value in health : the journal of the International Society for Pharmacoeconomics and Outcomes Research, 9(4), 272–274
8Coyne, K. S., et al. (2014). Economic burden of urgency urinary incontinence in the United States: a systematic review. Journal of managed care pharmacy : JMCP, 20(2), 130–140.
9Ganz, M. L., et al. (2010). Economic costs of overactive bladder in the United States. Urology, 75(3), 526-532.
10Wagg, A., et al. (2012). Persistence with prescribed antimuscarinic therapy for overactive bladder: a UK experience. BJU international, 110(11), 1767–1774.
0